- Schedule an Appointment Today
- (310) 231-5100
- drjelisha@gmail.com
Temporomandibular Joint Disorders (TMD, TMJ)
What Is TMJ Los Angeles?
December 18, 2019What Temporomandibular Joint (TMJ) Exercises Relieve Pain?
December 20, 2019
Problems with your jaw and the muscles in your face that control it are known as temporomandibular disorders (TMD). But you may hear it wrongly called TMJ, after the joint.
What Causes TMD?
We don’t know what causes TMD. Dentists believe symptoms arise from problems with the muscles of your jaw or with the parts of the joint itself.
Injury to your jaw, the joint, or the muscles of your head and neck — like from a heavy blow or whiplash — can lead to TMD. Other causes include:
What Are the Symptoms?
TMD often causes severe pain and discomfort. It can be temporary or last many years. It might affect one or both sides of your face. More women than men have it, and it’s most common among people between the ages of 20 and 40.
Common symptoms include:
- Pain or tenderness in your face, jaw joint area, neck and shoulders, and in or around the ear when you chew, speak, or open your mouth wide
- Problems when you try to open your mouth wide
- Jaws that get “stuck” or “lock” in the open- or closed-mouth position
- Clicking, popping, or grating sounds in the jaw joint when you open or close your mouth or chew. This may or may not be painful.
- A tired feeling in your face
- Trouble chewing or a sudden uncomfortable bite — as if the upper and lower teeth are not fitting together properly
- Swelling on the side of your face
How Is TMD Diagnosed?
Many other conditions cause similar symptoms — like tooth decay, sinus problems, arthritis, or gum disease. To figure out what’s causing yours, the dentist will ask about your health history and conduct a physical exam.
He’ll check your jaw joints for pain or tenderness and listen for clicks, pops, or grating sounds when you move them. He’ll also make sure your jaw works like it should and doesn’t lock when you open or close your mouth. Plus he’ll test your bite and check for problems with your facial muscles.
Your dentist may take full face X-rays so he can view your jaws, temporomandibular joints, and teeth to rule out other problems. He may need to do other tests, like magnetic resonance imaging (MRI) or computer tomography (CT). The MRI can show if the TMJ disc is in the proper position as your jaw moves. A CT scan shows the bony detail of the joint.
You may get referred to an oral surgeon (also called an oral and maxillofacial surgeon) for further care and treatment. This doctor specializes in surgery in and around the entire face, mouth, and jaw area. You may also see an orthodontist to ensure your teeth, muscles, and joints work like they should.
Home Treatments for TMD
There are things you can do on your own to help relieve TMD symptoms. Your doctor may suggest you try some of these remedies together.
Take over-the-counter medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), like naproxen or ibuprofen, can relieve muscle pain and swelling.
Use moist heat or cold packs. Apply an ice pack to the side of your face and temple area for about 10 minutes. Do a few simple jaw stretches (if your dentist or physical therapist OKs them). When you’re done, hold a warm towel or washcloth to the side of your face for about 5 minutes. Perform this routine a few times each day.
Eat soft foods. Add yogurt, mashed potatoes, cottage cheese, soup, scrambled eggs, fish, cooked fruits and vegetables, beans, and grains to your menu. Cut foods into small pieces so you chew less. Skip hard, crunchy foods (like pretzels and raw carrots), chewy foods (like caramels and taffy), and thick or large bites that require you to open wide.
Don’t rest your chin on your hand. Don’t hold the phone between your shoulder and ear. Practice good posture to reduce neck and facial pain.
Keep your teeth slightly apart as often as you can. This will relieve pressure on your jaw. Put your tongue between your teeth to control clenching or grinding during the day.
Learn relaxation techniques to help loosen up your jaw. Ask your dentist if you need physical therapy or massage. Consider stress reduction therapy as well as biofeedback.
Traditional Treatments
Talk to your dentist about these tried-and-true treatments for TMD:
Medications. Your dentist can prescribe higher doses of NSAIDs if you need them for pain and swelling. He might suggest a muscle relaxer to relax your jaw if you grind or clench your teeth. Or an anti-anxiety medication to relieve stress, which may bring on TMD. In low doses they can also help reduce or control pain. Muscle relaxants, anti-anxiety drugs, and antidepressants are available by prescription only.
A splint or night guard. These plastic mouthpieces fit over your upper and lower teeth so they don’t touch. They lessen the effects of clenching or grinding and correct your bite by putting your teeth in a more correct position. What’s the difference between them? You wear night guards while you sleep. You use a splint all the time. Your dentist will tell you which type you need.
Dental work. Your dentist can replace missing teeth and use crowns, bridges, or braces to balance the biting surfaces of your teeth or to correct a bite problem.
Other Treatments
If the treatments listed above don’t help, your dentist may suggest one or more of the following:
Transcutaneous electrical nerve stimulation (TENS). This therapy uses low-level electrical currents to provide pain relief by relaxing your jaw joint and facial muscles. It can be done at the dentist’s office or at home.
Ultrasound. Deep heat applied to the joint can relieve soreness or improve mobility.
Trigger-point injections. Pain medication or anesthesia is injected into tender facial muscles called “trigger points” to give relief.
Radio wave therapy. Radio waves stimulate the joint, which increases blood flow and eases pain.
Low-level laser therapy. This lowers pain and inflammation and helps you move your neck more freely and open your mouth wider.
Surgery for TMD
If other treatments can’t help you, surgery is an option. Once it’s done, it can’t be undone, so get a second or even third opinion from other dentists.
There are three types of surgery for TMD. The type you need depends on the problem.
Arthrocentesis is used if you have no major history of TMJ but your jaws are locked. It’s a minor procedure that your dentist can do in his office. He’ll give you general anesthesia, then insert needles into the joint and wash it out. He may use a special tool to get rid of damaged tissue or dislodge a disc stuck in the joint, or to unstick the joint itself.
Arthroscopy is surgery done with an arthroscope. This special tool has a lens and a light on it. It lets your doctor see inside your joint. You’ll get general anesthesia, then the doctor will make a small cut in front of your ear and insert the tool. It’ll be hooked up to a video screen, so he can examine your joint and the area around it. He may remove inflamed tissue or realign the disc or joint. This type of surgery, known as minimally invasive, leaves a smaller scar, has fewer complications, and requires a shorter recovery time than a major operation.
- The bony structures in your jaw joint are wearing down
- You have tumors in or around the joint
- Your joint is scarred or full of bone chips
You’ll get general anesthesia, then the doctor will open up the entire area around the joint so he can get a full view and better access. You’ll need longer to heal after open-joint surgery, and there is a greater chance of scarring and nerve injury.
TMJ Specialist Los Angeles
Dr. Jacob Elisha has over 30 years of experience in the field of dentistry, periodontics, and cutting-edge restorative techniques in Los Angeles, CA. Dr. Jacob Elisha is an authority in on TMJ Disorders. He has successfully treated patients with TMJ disorders in Los Angeles in the past and looks forward to the future.
TMJ Disorders. An award-winning oral maxillofacial surgeon and Los Angeles TMJ specialist, Dr. Jacob Elisha is known for providing among the most effective TMJ treatment Beverly Hills has to offer—improving jaw function and delivering permanent relief from chronic pain.
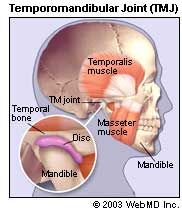
TMJ disorders affect your temporomandibular joint, which allows your mouth to open and move smoothly. We offer specialized treatment in Los Angeles, CA . The temporomandibular (tem-puh-roe-man-DIB-u-lur) joint (TMJ) acts like a sliding hinge, connecting your jawbone to your skull. You have one joint on each side of your jaw. TMJ disorders — a type of temporomandibular disorder or TMD — can cause pain in your jaw joint and in the muscles that control jaw movement. The exact cause of a person’s TMJ disorder is often difficult to determine. Your pain may be due to a combination of factors, such as genetics, arthritis or jaw injury. Some people who have jaw pain also tend to clench or grind their teeth (bruxism), although many people habitually clench or grind their teeth and never develop TMJ disorders. In most cases, the pain and discomfort associated with TMJ disorders is temporary and can be relieved with self-managed care or nonsurgical treatments. Surgery is typically a last resort after conservative measures have failed, but some people with TMJ disorders may benefit from surgical treatments. TMJ disorders can also cause a clicking sound or grating sensation when you open your mouth or chew. But if there’s no pain or limitation of movement associated with your jaw clicking, you probably don’t need treatment for a TMJ disorder. Seek medical attention if you have persistent pain or tenderness in your jaw, or if you can’t open or close your jaw completely. Your doctor, your dentist or a TMJ specialist can discuss possible causes and treatments for your problem.
What are the risk factors for TMJ syndrome? There are several risk factors for TMD: Poor posture in the neck and upper back muscles may lead to neck strain and abnormalities of jaw muscle function. Stress may increase muscle tension and jaw clenching. Women 18-44 years of age have increased risk. Patients with other chronic inflammatory arthritis have increased risk. People with jaw trauma or poorly positioned teeth have increased risk. People who have a genetic predisposition to pain sensitivity and increased stress responses may be more susceptible.
The temporomandibular joint is more commonly referred to as the TMJ joint, but what is TMJ? This joint is actually located at the base of the skull in front of the ear structure and connects the lower jaw (mandible) with the upper jaw (maxilla). Unlike most joints located in the body, the TMJ is unique in its structure, composed of a rounded protrusion of the mandible that sits against an indentation in the skull, and a disc-like structure made of a soft bone called cartilage found in between the two bones (articular disc). These three parts of the TMJ are held together by ligaments originating from different parts of the head and neck to support the jaw and guide its movements. Several muscles are connected to those ligaments, and many aid in the motion of the lower jaw. How Does it Work? The TMJ works in two ways to open your mouth: The first way is like a hinge to simply open and close the mouth, just like a hinge on a door. The second way is a sliding motion called translation, wherein your lower jaw moves down and forward. This motion helps the TMJ to move backward and forward and from side to side for actions such as eating, yawning and singing – some of the most common. What Can Happen to the TMJ? Like any other joint in the body, the TMJ can be fractured, swell and become sore, causing limited movement of the lower jaw and pain radiating to the head and neck area. A fracture to the actual articular disc is rare, but it can be displaced, causing severe pain and swelling. Unlike other joints such as knees and hips, arthritis of the TMJ is very rare, and hard to treat with anti-inflammatory drugs alone. Nonetheless, pain in the TMJ is often temporary, and can be treated with a combination of ice then heat to relieve the sore ligaments and muscles surrounding the joint. The temporomandibular joint (TMJ) is the joint that connects the jaw to the temporal bones of the skull. Temporomandibular joint disorder, known more commonly as TMD, occurs when there are problems with the muscles and jaws in the face. There are many signs and symptoms of TMD. It’s often hard to know for sure if you have TMD, because one or all of these symptoms can also be present for other problems. Your dentist can help make a proper diagnosis. What About Grinding and Clenching? Sometimes, pain in the TMJ can come from the teeth themselves, as opposed to the TMJ and surrounding ligaments.
As a TMJ doctor, Dr. Jacob Elisha delivers a TMJ treatment in Los Angeles for patients who are suffering from extreme pain to help resolve the condition. Because TMJ disorders can be extremely painful, Dr. Jacob Elisha’s first priority is symptom relief. Although these measures won’t permanently cure TMJ, they will alleviate much of the chronic pain associated with the condition. This variety makes diagnosis and treatment challenging. An accurate diagnosis is critical for successful treatment. For instance, patients with a muscle problem that is causing pain will most likely not benefit from surgery on the temporomandibular joint (TMJ). Ask about your doctor’s experience in diagnosing and treating TMJ and facial pain. Most problems, whether muscular or within the joint, get better over time. For this reason, most experts agree that it’s best to use conservative treatment at first. But in some instances, surgery or other procedures, such as injections, may be recommended as a first treatment. Most people with TMD have temporary symptoms that are not serious and do not get worse. They usually can get better with simple treatments done at home. Sometimes symptoms go away without any treatment at all. They also can come back without warning. If you have TMD, your dentist may suggest the treatments listed below. Most dentists agree that these treatments work best in combination. You may not get relief using only one. To begin, Dr. Jacob Elisha will prescribe a pain reliever, anti-inflammatory or muscle relaxant to relieve muscle spasms and joint pain. In some cases, he may also inject a specialized steroid directly into the joints to dramatically reduce pain and inflammation. From there, Dr. Jacob Elisha will prescribe self-care treatments—advising the patient to rest the jaw, eat soft foods, apply ice to the affected area and practice proper posture. Depending on the specifics of your TMJ disorder, he may also recommend physical therapy to improve jaw function.
